
The Merrick Lab

Institute for Diabetes, Obesity, and Metabolism
Overview
Adipose mesenchymal progenitors represent a complex pool of highly diverse cell types, for which we utilize unbiased techniques such as single-cell RNA transcriptomics to identify novel subpopulations of adipocyte progenitors from subcutaneous fat including Dpp4+ interstitial progenitor cells and Icam1+ committed preadipocytes. Dpp4+ progenitors demonstrate many properties classically attributed to mesenchymal stem cells including enhanced proliferative and multilineage differentiation potential. Icam1+ cells appear to be committed to the adipocyte lineage and are poised to undergo adipogenesis with minimal stimulation. Using cell transplantation and lineage tracing approaches, we have established a lineage hierarchy in which Dpp4+ cells serve as upstream progenitors that give rise to Icam1+ preadipocytes and mature adipocytes. Importantly, we found that the same cell populations and lineage relationships are present in human subcutaneous adipose. Adipocyte progenitor dysfunction, leading to inadequate de novo adipogenesis is thought to represent one of the main mechanisms contributing to the metabolic consequences of obesity. Therefore, understanding the physiological role of Dpp4+ and Icam1+ progenitor cells and how they are disrupted in the setting of obesity is of paramount importance. While the prevailing dogma in the field states that adipocyte progenitors are located in the perivascular space, we discovered that Dpp4+ progenitors reside in a previously unrecognized anatomic niche which we termed the Reticular Interstitium (RI), a previously overlooked connective tissue that envelops many organs. Furthermore, Dpp4+ progenitors cells demonstrated robust multilineage potential to differentiate into osteocytes and chondrocytes. The multipotent nature of Dpp4+ cells and their ubiquitous distribution throughout the body supports the hypothesis that, in addition to serving as precursors for adipocytes, these cells may play an important role in the development, regeneration and fibrosis of other mesenchymal tissues.
Current Projects
In vivo lineage tracing of Dpp4+ interstitial progenitor cells
Adipose mesenchymal progenitors represent a complex pool of highly diverse cell types, for which we utilize unbiased techniques such as single-cell RNA transcriptomics to identify novel subpopulations of adipocyte progenitors from subcutaneous fat including Dpp4+ interstitial progenitor cells and Icam1+ committed preadipocytes. Dpp4+ progenitors demonstrate many properties classically attributed to mesenchymal stem cells including enhanced proliferative and multilineage differentiation potential. Icam1+ cells appear to be committed to the adipocyte lineage and are poised to undergo adipogenesis with minimal stimulation. Using cell transplantation and lineage tracing approaches, we have established a lineage hierarchy in which Dpp4+ cells serve as upstream progenitors that give rise to Icam1+ preadipocytes and mature adipocytes. Importantly, we found that the same cell populations and lineage relationships are present in human subcutaneous adipose. Adipocyte progenitor dysfunction, leading to inadequate de novo adipogenesis is thought to represent one of the main mechanisms contributing to the metabolic consequences of obesity. Therefore, understanding the physiological role of Dpp4+ and Icam1+ progenitor cells and how they are disrupted in the setting of obesity is of paramount importance.
Current projects are focused on testing the hypothesis that Dpp4+ progenitors give rise to Icam1+ committed preadipocytes and mature adipocytes in vivo during both embryologic adipose organogenesis and in the setting of stimulated adipogenesis in the adult; and that Dpp4+ progenitors may contribute to adipose fibrosis in the setting of high fat diet-induced obesity. To assess the role of endogenous Dpp4+ progenitor cells during adipogenesis in vivo, we have generated lineage tracing mice that leverage the specific expression of Dpp4 in the mesenchymal progenitor cells. We are using the Dpp4CreER model to track the fate of interstitial progenitor cells and their progeny as they progress through the stages of adipocyte or alternative fate commitment. Interstitial progenitor cells display many characteristics classically associated with traditional fibroblasts including the expression of collagen, fibronectin and matrix modulating genes. This gene pattern may reflect their likely role in maintaining the collagenous interstitium in which they normally reside, however these properties could also contribute to pathologic fibrosis if the Dpp4+ progenitors become activated in an ectopic location such as the parenchyma of the adipose tissue.
While the prevailing dogma in the field states that adipocyte progenitors are located in the perivascular space, we discovered that Dpp4+ progenitors reside in a previously unrecognized anatomic niche which we termed the Reticular Interstitium (RI), a previously overlooked connective tissue that envelops many organs. Furthermore, Dpp4+ progenitors cells demonstrated robust multilineage potential to differentiate into osteocytes and chondrocytes. The multipotent nature of Dpp4+ cells and their ubiquitous distribution throughout the body supports the hypothesis that, in addition to serving as precursors for adipocytes, these cells may play an important role in the development, regeneration and fibrosis of other mesenchymal tissues.

Function of Pi16 protein
The Merrick Lab has generated a murine Pi16-KO line. An upcoming project in the lab is to investigate the function of the protein Pi16 in vivo.
WT

KO

Characterization of reticular interstitium resident Lyve1+ macrophages
The reticular interstitium represents a previously under-recognized anatomical niche for progenitor cells and, despite its potentially exciting role as a stem cell reservoir, the RI and its resident fibroblastic progenitors have only recently begun to receive intense scientific interest. We employed unbiased single cell RNA-sequencing to reveal that the RI is cohabited by Dpp4+ mesenchymal progenitors, as well as a unique population of macrophages marked by the expression of Lyve1. The close anatomic proximity of these two cell populations within the RI strongly suggests that Lyve1+ macrophages participate in immune-cell crosstalk with Dpp4+ cells and express niche defining elements that regulate Dpp4+ progenitor activity. Furthermore, we discovered a dramatic shift in the macrophage transcriptional profile in the setting of obesity: lean adipose contains pro-adipogenic macrophages; while obese adipose demonstrate a large influx of Cd9+ macrophages that are reportedly anti-adipogenic. These findings support the overarching hypothesis that Dpp4+ progenitors entering lean adipose encounter a pro-adipogenic macrophage signaling environment that is conducive to de novo adipogenesis, while Dpp4+ progenitors recruited into obese adipose tissue are met with anti-adipogenic/ pro-inflammatory Cd9+ macrophages, which might direct them into a fibrotic myofibroblast cell fate. We are actively investigating this hypothesis using FACS and single-cell to uncover candidate receptor-ligand gene set relationships existing between the Dpp4+ progenitors and Lyve1+ macrophages. We have developed an inducible in vivo macrophage depletion model to examine the functional consequences of Dpp4+ immune cell crosstalk as it relates to adipogenesis and fibrosis.

Development and function of intramuscular adipose tissue
Millions of Americans experience both acute and chronic skeletal muscle injury, which displays an impressive ability to regenerate following injury. In certain contexts, muscle regeneration is accompanied by the formation of intramuscular adipose tissue (IMAT), a depot of adipocytes found between the fibers of skeletal muscle. IMAT is not typically found in large quantities in a healthy muscle; rather, it only appears in response to an external stimulus such as injury or obesity. Because IMAT is correlated with these external stimuli it has been assumed that the presence of IMAT is harmful for the muscle tissue. However, the precise role of IMAT remains unclear. Intramuscular adipocytes may form as an acute adaptive response to injury with the purpose of promoting muscle regeneration, but may also become maladaptive in chronic settings and impede muscle function.
Adipocytes that comprise IMAT arise from mesenchymal progenitor cells known as fibroadipogenic progenitors (FAPs). These FAPs reside within uninjured muscle tissue and, like other tissue-resident fibroblast populations throughout the body, are marked by expression of platelet-derived growth factor receptor alpha (Pdgfra). FAPs possess adipogenic but not myogenic differentiation capabilities and provide support to satellite cells, which are myogenic progenitors. In addition to a support role, FAPs isolated from muscle tissue display robust adipogenesis in vitro and directly contribute to IMAT formation in vivo. Loss of Pdgfra+ FAPs alone is sufficient to significantly impair muscle regeneration. Despite a propensity for adipogenesis, FAP differentiation to form IMAT does not occur spontaneously, suggesting that the healthy muscle tissue environment provides inhibitory signals to FAPs to prevent their differentiation into adipocytes. Upon external stimulus such as injury, this inhibition is perturbed and FAPs are allowed to differentiate and form IMAT. However, the signals that promote adipogenesis and the precise role that mature adipocytes play in the regenerative process remain unknown. Given this complex interplay between muscle fibers, FAPs, and adipocytes, we hypothesize that proper muscle regeneration following injury is dependent on crosstalk among all three cell types, and that regeneration is ultimately regulated by mature adipocytes.
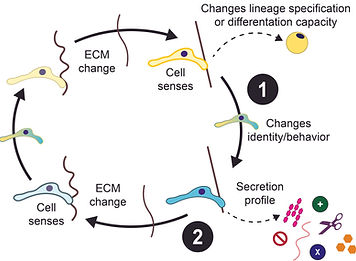
Understanding the mechanochemical environment of adipose tissue in obesity
Adipose tissue plays a crucial role in the body by storing nutrients, thereby protecting other tissues from nutrient excess. To accommodate influx, adipose tissue undergoes expansion, which necessitates a restructuring of the environment to allow for growth; namely, remodeling the structural component of tissue: the extracellular matrix (ECM). However, when this system is overwhelmed by chronic nutrient consumption, important equilibriums are lost, leading to expansion failure, adipose tissue dysfunction, and the negative consequences of obesity. Prior studies have shown alterations to ECM deposition and composition in obesity. Our single cell RNA-sequencing data from adipose tissue of lean and obese mice revealed differential ECM-related gene expression between different subpopulations of adipocyte progenitor cells (APCs) and macrophages and in obese versus lean mice. These data also point to a role for hyaluronic acid (HA) — a major structural component of the ECM that has important roles in cell communication, cell localization, inflammation, and tissue mechanics (such as its role in the joints as a lubricant). While alterations to the ECM and HA have been demonstrated in obesity, the consequences of these changes for tissue mechanics and cell behavior and what that means for adipose tissue expansion failure and dysfunction in obesity remain poorly understood.
The overall objective of this proposal is to address two knowledge gaps: (1) how cells respond to and communicate physical changes in the adipose tissue environment and (2) how cells modify their environment to accommodate expansion and how this fails in the context of obesity.

Investigating adipocyte development in the dermis
To investigate the process of adipocyte formation, we performed single-cell RNA sequencing of Pdgfra+ pre-adipocytes in C57BL6 mouse embryos at timepoints prior to the start of adipogenesis (e12) through the formation of mature adipocytes (e16). A cluster of cells marked by Bcl11b showed strong expression at the e14 timepoint but dramatically decreased expression by e15 and e16. IHC staining revealed Bcl11b+ cells are localized to the dermis and co-expressed with Pdgfra+ cells.
To study the role of Bcl11b+ cells in adipocyte development, we generated PdgfraCre / Bcl11bflox/flox mice to constitutively knockout Bcl11b in pre-adipocytes. Bcl11b-KO mice had little to no adipocytes in their dermis at post-birth day 6 compared to wild-type controls. Adipocyte development in the subcutaneous iWAT was unaffected by the Bcl11b-KO.

e14

Sorted pre-adipocytes from the iWAT and skin of control and Bcl11b-KO mice were plated and given a strong induction cocktail in vitro to induce adipogenesis. ICAM1+ pre-adipocytes, which are highly committed to becoming mature adipocytes, were largely unable to differentiate even when removed from the in vivo environment of the Bcl11b-KO mouse dermis. Pre-adipocytes from the Bcl11b-KO iWAT, where no Bcl11b is present at e14, were unaffected by the knockout and were able to differentiate as normal. The Merrick Lab will continue to investigate the role of Bcl11b in dermal adipogenesis by conducting ChIP seq and other experiments using in vitro and in vivo models.


Brown adipose tissue as a therapeutic for metabolic syndrome
The Merrick Lab, in coordination with The University of Pennsylvania’s Stem Cell and Xenograft Core and Human Metabolic Tissue Bank, is utilizing donated human-derived adipose stem cells to study brown and beige adipocyte differentiation. Current projects include the development of serum-free media to use in vitro, xenograft generation in NSG and nude mice, and exciting optogenetic experiments to test the therapeutic potential of brown adipose tissue to ameliorate metabolic disease.












